Today one of my favorite authors published a new study. His name is Mathew Walker, Ph.D. He, along with several of his colleagues from University of California, Berkley have been studying sleep patterns in patients which may predict the onset of Alzheimer’s disease. They appear to be on to some very important findings.
Before describing the study, I’d like to put in a plug for Dr. Mathew Walker’s book, Why We Sleep: Unlocking the Power of Sleep and Dreams. This was a New York Times best seller. This book is the best I’ve read about the significance of sleep and its deep and broad impacts on health. It’s easy to read, not a textbook but well referenced. Dr. Walker is an excellent writer who has a very engaging style. Everyone who is concerned about maximizing their health potential should read this book. Essentially, if you have a brain and want to take care of it well, I recommend reading his book!
Back to the study. It suggests that sleep patterns predicted the levels of pathologic Alzheimer’s proteins (tau and amyloid-beta) in the brains of cognitively normal older adults. Wow! These were normal older people and just looking at their sleep EEG patterns could predict the accumulation of these pathologic proteins.
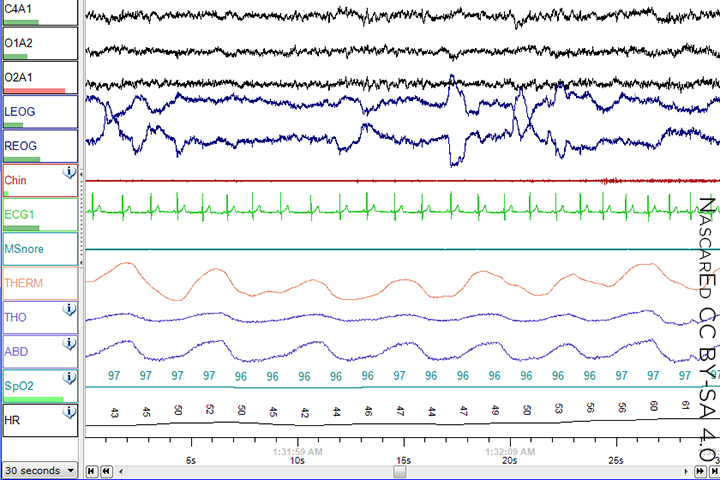
What were the specifics? A decrease in the slow oscillations and sleep spindle synchronization on EEG sleep recordings was linked with higher tau. While reduced slow wave amplitude was tied with higher Aβ levels.
Here’s another important finding. Changes in sleep duration which occurred over preceding decades also predicted Aβ and tau burden later in life.
The final take-home from this study is that polysomnography testing (aka, a sleep study) could offer a window into uncovering sleep deficiencies earlier in life. Correcting these deficiencies could prevent or delay Alzheimer’s disease progression later in life.
A deeper dive into sleep… From an EEG viewpoint, sleep is divided into two major types. REM, or rapid eye movement and non-REM. REM is where dreaming occurs. The body is paralyzed except for the eyes which exhibit these rapid movements. REM is definitely involved in the process of laying down new memories. Non-REM, is divided into multiple sub-types. One of these goes by various names; deep, delta, or slow-wave sleep. This is the deepest sleep where it is most difficult to arouse a person from and is responsible for a myriad of restorative processes in the body and the brain. One of these, it would appear, is the clearance of accumulated proteins such as amyloid-β and tau. The EEG during slow wave sleep exhibits two characteristic features; slow oscillations, for which it gets its name, as well as sleep spindles. If the architecture of these two features become uncoordinated, which occurs frequently with aging, that is associated with the development of AD pathology. And, it’s important to point out once again that these changes are happening decades (how many we don’t know) before the development of cognitive decline.
In this study the researchers used polysomnography and retrospective questionnaires to study 101 cognitively normal adults. These patients had concurrent PET and MRI data available. And a subset of 31 completed a sleep EEG assessment while 95 completed the questionnaire about lifespan sleep duration and sleep quality change.
The EEG data showed that the severity of impaired slow oscillation-sleep spindle coupling predicted greater medial temporal lobe tau burden. The coupling impairment was specific to tau accumulation with no association to Aβ burden.
Meanwhile, a non-REM EEG signature of impaired 0.6-1 Hz slow-wave activity predicted cortical Aβ, but not tau accumulation.
Looking at the questionnaire data collected it appears that sleep patterns across life are associated with and predict later in life Aβ and tau burden. The authors state “This finding may suggest that decreasing sleep duration in mid to late life is significantly associated with an increased risk of late-life Aβ burden.” And, more reassuringly stated, “that a profile of maintained (or even subtle increase) in sleep duration throughout this period is statistically associated with a reduced predicted risk of Aβ accumulations in late life.”
Limitations of the study. This was a small sample size and there could be subjective bias. Larger studies are needed to confirm the findings. However, it would appear that if valid, these results would have great importance for public health in terms of Alzheimer’s disease prevention.
In our practice, we take a very pro-active approach to sleep. We ask detailed questions about sleep quality from our patients both in person, as well as scientifically validated forms. We will not hesitate to recommend a sleep study if there is any question that poor sleep may be a factor for an individual. And we have developed many strategies to combat the epidemic of poor sleep. Current estimates are that 35% of Americans that currently are lacking sufficient sleep.
Alzheimer’s disease is the sixth leading cause of death in the U.S. with 5.7 million Americans currently living with the condition. While there is no cure, prevention and early diagnosis are crucial to slow the progression of the disease. We are currently using a state of the science clinically proven model called ReCODE(TM) in order to address the many factors which contribute to the development of cognitive decline. Using such a comprehensive, programmatic approach to workup and treatment can significantly improve the odds when it comes to both treatment and prevention.
Source Reference: Winer J, et al “Sleep as a potential biomarker of tau and β-amyloid burden in the human brain” J Neurosci 2019; DOI: 10.1523/JNEUROSCI.0503-19.2019.