Can poor sleep place you at risk for developing Alzheimer’s disease?
Not surprisingly, the answer is “yes.” Certainly, everyone recognizes the importance of good sleep! There is seemingly no aspect of life, or health not impacted by sleep. If it were a medication, sleep would be the most successful drug ever created.
For years now, researchers have noted poor sleep is linked to Alzheimer’s disease. Now, the mechanisms are becoming quite clear. The first clue came as patients with Alzheimer’s displayed uniformly poorer sleep quality than unaffected individuals. Moreover, it seemed the worse their sleep, the worse the disease tended to be. Recently, it has become clear the linkage is bi-directional (1-3). Not only does Alzheimer’s cause poor sleep, but poor sleep may cause Alzheimer’s. By studying patients at risk of developing Alzheimer’s, researchers have discovered that sleep disturbances precede the development of clinical symptoms of the disease, surprisingly by as much as 15 years! Moreover, the pathological correlates of Alzheimer’s disease, namely amyloid-β plaques and tau protein tangles, are directly affected by sleep.
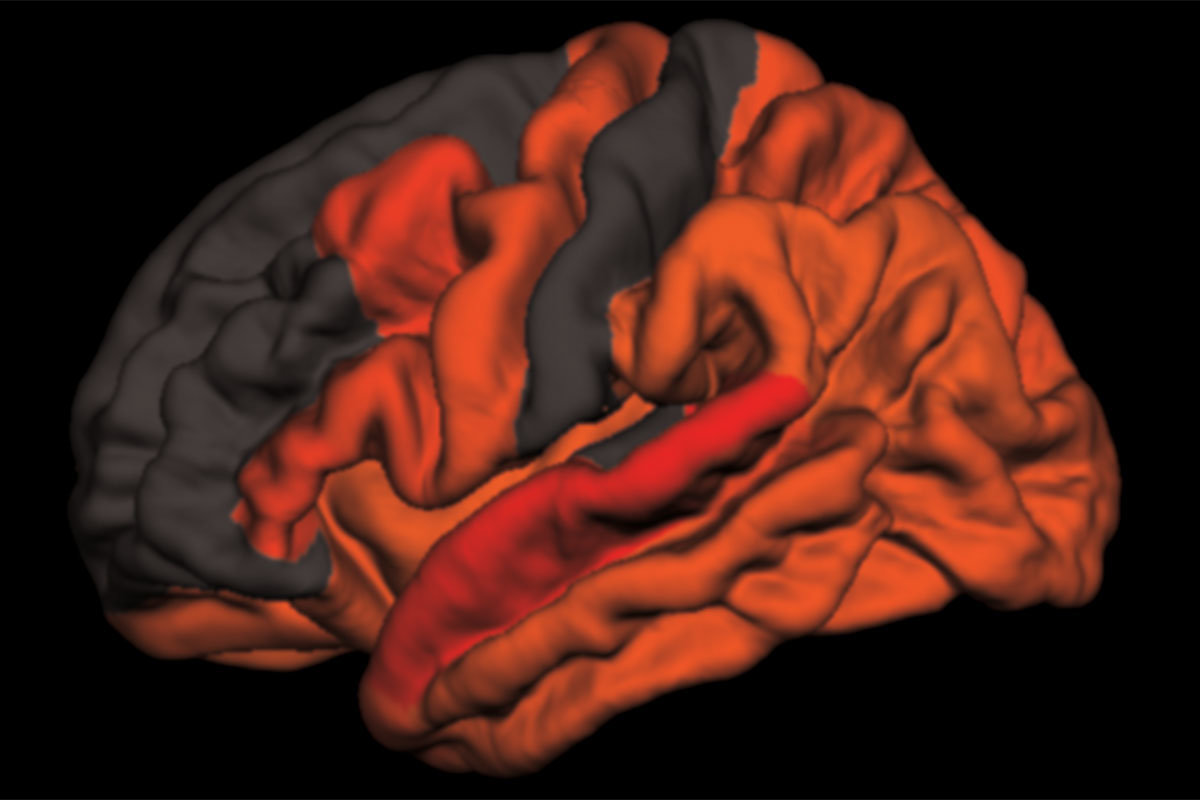
Researchers at Washington University in St. Louis believe they have uncovered part of the explanation. According to research published January 9, 2019 in the journal Science Translational Medicine, poor sleep quality in later life is linked to the accumulation of tau protein in the brain. (4) The type of sleep involved was deep sleep. You may recall hearing about REM (Rapid Eye Movement) sleep. That’s where dreaming occurs. Deep sleep is sort of the opposite of REM. Instead of fast brain wave activity (almost like being awake), deep sleep is associated with unique feature of slow waves (also called delta-waves) on EEG (electro-encephalogram, or brain wave monitoring). A lot of interesting things happen in deep sleep. Beyond the scope of this article! But suffice it to say, decreased slow wave sleep activity correlated with increased deposits of both amyloid and tau proteins. (4) This protein debris is cleared away during deep (slow wave) sleep. As little as one night of sleep disruption will increase the accumulation of these proteins. Even worse, the more build-up, the worse sleep becomes, accelerating the decline.
Multiple factors may affect sleep, and hence Alzheimer’s disease pathology. These include age, sex, ApoE4 status, family history and various sleep disorders. Self-reported poor sleep quality is certainly a factor. But often times, can be difficult to appreciate because changes to our sleep develop slowly over time and it’s difficult for an individual to objectively measure his or her sleep. The time spent asleep is definitely important. We know that this changes over time with age. Older individuals are noted to have shorter sleep than say, adolescents or people in their twenties. However, is this natural, or is it the effect of accumulating damage to the brain? We’re starting to wonder if it may be the latter. It certainly seems to fit that shorter sleep over time may be one of the key aspects involved in brain aging and loss of cognitive function in older adults.
We take this association between sleep and cognitive decline very seriously in our clinic. We dialogue extensively with our patients seeking to understand their sleep habits. We use scientifically validated instruments to uncover hidden sleep issues. And if we find any concerns, don’t hesitate to order further appropriate studies to clarify these issues. Sleep is one of the most fundamentally important aspects of wellness across all dimensions of life. Rest assured, we have expertise in ways to optimize your sleep and help prevent, or reverse negative effects on your health both cognitively and otherwise. Stay tuned to the blog as we’ll have more articles about how to optimize sleep for health.
- Y.-E. Ju, B. P. Lucey, D. M. Holtzman, Sleep and Alzheimer disease pathology— A bidirectional relationship. Nat. Rev. Neurol. 10, 115–119 (2014).
- B. P. Lucey, R. J. Bateman, Amyloid-diurnal pattern: Possible role of sleep in Alzheimer’s disease pathogenesis. Neurobiol. Aging 35, S29–S34 (2014).
-
E. S. Musiek, D. M. Holtzman, Mechanisms linking circadian clocks, sleep, and neurodegeneration. Science 354, 1004–1008 (2016).
4. B. P. Lucey, A. McCullough, E. C. Landsness, C. D. Toedebusch, J. S. McLeland, A. M. Zaza, A. M. Fagan, L. McCue, C. Xiong, J. C. Morris, T. L. S. Benzinger, D. M. Holtzman, Reduced non– rapid eye movement sleep is associated with tau pathology in early Alzheimer’s disease. Sci. Transl. Med. 11, eaau6550 (2019).